Having a Thoracic Epidural Injection
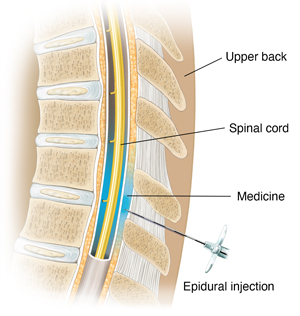
A thoracic epidural injection is a shot that helps ease pain in your upper to middle back (thoracic) area. Medicine is injected into the area around your spinal cord.
What to tell your health care provider
Tell your provider about all the medicines you take. This includes over-the-counter medicines, such as ibuprofen. It also includes vitamins, herbs, and other supplements. And tell your provider if you:
-
Have had any recent changes in your health, such as an infection or fever.
-
Are sensitive or allergic to contrast dye.
-
Are sensitive or allergic to any medicines, latex, tape, or anesthesia (local and general).
-
Are pregnant or think you could be.
Tests before your procedure
You may need other tests before you get the injection. For example, you may have an MRI scan of your upper to middle back area.
Getting ready for your procedure
Talk with your health care provider about how to get ready for your procedure. You may need to stop taking some medicines before the procedure, such as blood thinners and aspirin.
Also, make sure to:
-
Ask a family member or friend to take you home from the hospital or outpatient facility.
-
Not eat or drink for several hours before your procedure.
-
Follow all other instructions from your provider.
You will be asked to sign a consent form that gives your provider permission to do the procedure. Read the form carefully. Ask questions if something isn't clear.
On the day of your procedure
You may have the procedure at the hospital, a surgery center, or a clinic. A pain specialist, radiologist, or other type of specialist may do the procedure. Your health care provider can tell you exactly what to expect. In general:
-
You may be given medicine to make you feel relaxed and sleepy (sedation).
-
You will lie on your belly (abdomen) or on your side on a special table.
-
The provider will clean the skin on your back in the area of the injection.
-
They will inject some medicine to numb the area (local anesthetic).
-
The provider will use special X-ray (fluoroscopy or CT scan) to put the needle into the correct area.
-
They will inject contrast dye to make sure the needle is in the epidural space.
-
They will slowly inject medicine. It's usually a mix of anti-inflammatory medicine (steroid) and numbing medicine (anesthetic). You may feel slight discomfort and pressure.
-
When done, the provider will remove the needle. They may cover the injection site with a small bandage.
-
The steroid medicine reduces swelling and nerve irritation. The anesthetic medicine numbs the area.
After your procedure
After the procedure, you will be moved to a chair or bed to rest for a while. The health care staff will watch you for any problems. You should be able to go home in an hour or so. Make sure to follow all directions from your health care provider and the staff. You may be told to:
-
Rest for the rest of the day, and go back to your normal activities the next day.
-
Not drive or make any important decisions for at least 24 hours, if you had sedation.
-
Expect some numbness in your arms that will go away within a few hours.
Recovering at home
You may not notice any improvement right after the injection. You may even feel a little worse afterward. It may take a few days to a week until you have less pain. The pain relief may last for weeks or months. Or the pain may not return at all. Sometimes no pain relief occurs.
Follow-up care
You’ll have an appointment with your health care provider in 1 to 2 weeks, or as advised by your provider, to discuss:
-
If the injection has reduced your pain.
-
If you need more injections.
-
Other treatment you may need, such as exercises, medicines, and physical therapy.
When to get medical advice
Contact your health care provider right away if you have:
-
A fever of 100.4°F (38°C) or higher, or as advised by your provider.
-
Numbness at the injection site that doesn’t go away.
-
Warmth and redness at the injection site, or in your arms, that doesn't go away.
-
Pain that is getting worse.